Coronary Artery Spasm
Coronary artery spasm is a cause of angina. Angina is pain that is caused when the heart muscles don't get enough blood and oxygen. A sudden spasm or narrowing of a coronary artery (blood vessel that supplies blood and oxygen back to the heart) can cause angina. This often causes pain. Sometimes severe spasms can lead to irregular heartbeats. They can even cause a heart attack and sudden death. Coronary artery spasm is also called vasospastic, variant, or Prinzmetal angina.
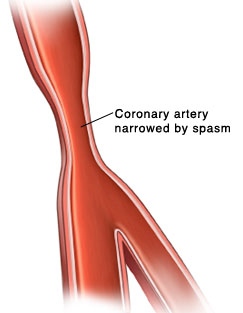 |
| Coronary artery spasm occurs when the wall of an artery contracts suddenly, narrowing the artery. |
How is a coronary artery spasm different from other anginas?
This condition differs from other types of angina. Other types of angina commonly occur when the person is active. They also tend to occur in people with coronary artery disease (CAD). With CAD, arteries in the heart have a buildup of a fatty substance called plaque. The plaque narrows the coronary arteries and reduces blood flow to the heart muscle, which causes angina. Angina with CAD is often brought on by an increased workload on the heart muscle, such as during exercise. In contrast, coronary artery spasm most often occurs during rest. In fact, it often occurs at night during sleep, often between midnight and early morning.
Symptoms of coronary artery spasm
The main symptom is a squeezing, crushing, or burning feeling in the chest. It may be described as a "discomfort." It's temporary, often lasting 5 to 30 minutes. Loss of consciousness may also occur. In some cases, there are no symptoms (a “silent” spasm).
Risk factors for coronary artery spasm
Risk factors are things that make you more likely to have a certain condition. Coronary artery spasm has several key risk factors. These include:
But coronary artery spasm often occurs in people without these risk factors.
Triggers for coronary artery spasm
Triggers are things that can prompt a spasm. These can include:
-
Smoking
-
Use of stimulant medicines and drugs such as cocaine, some antimigraine medicines, and amphetamines
-
Changes in heart rate regulation by the nervous system
-
Magnesium deficiency
-
Emotional stress
-
Alcohol use
-
Exposure to cold
-
Migraines
-
Use of medicine that causes narrowing of the blood vessels
-
Undergoing heart procedures such as coronary angiogram and coronary artery stenting
-
Botulism, a bacteria that can be found in food
Diagnosis of coronary artery spasm
Your healthcare provider will take a health history and ask you to describe your symptoms. You’ll have a physical exam and certain tests may be done. These may include:
-
Electrocardiogram (ECG). This test records the electrical activity of your heart. An ECG can detect an abnormal pattern, particularly during the chest pain episode. It can also detect an irregular heart rhythm associated with coronary artery spasm.
-
Echocardiogram. This is an ultrasound of the heart that examines its valves, pumping mechanism, and blood flow. It can detect problems in heart strength and function.
-
Coronary angiography. This is a special type of X-ray that is part of a heart catheterization (cardiac cath). A long plastic tube (catheter) is inserted in an artery, usually in the groin or arm, and advanced to the heart. Then a special dye is injected into the coronary arteries to create pictures of these arteries. These pictures show any narrowing or blockage in these blood vessels. This is the gold standard for confirming the diagnosis of coronary artery spasm or coronary artery disease from plaque narrowing.
Treatment of coronary artery spasm
There are 2 main types of treatment or prevention for coronary artery spasm. They are medicine and lifestyle changes. Coronary spasm is not treated or prevented using bypass procedures or invasive procedures in the coronary arteries such as angioplasty or coronary artery stents.
If you are prescribed these or any other medicines, follow your healthcare provider’s instructions on how and when to take them.
-
Lifestyle changes can also help prevent spasms. Start by staying away from the triggers listed above. Also talk with your healthcare provider about what you can do to reduce your risk for CAD. This may include eating a healthy diet and starting an exercise plan. If you smoke, talk with your provider about ways to stop.
Signs of a heart attack
Because of your risk, you need to watch for signs of heart attack. Don’t be afraid to call911, even if you’re not sure you are having a heart attack. Never drive yourself to the hospital if you think you are having a heart attack because of the risk of losing consciousness and causing an accident. Below are some common symptoms of heart attack:
-
Pressure, squeezing, or pain in your chest, neck, jaw, shoulders, arms, or back
-
Severe shortness of breath
-
Dizziness or faintness
-
Nausea and vomiting
-
Rapid or irregular heartbeat
-
Sweating
-
Indigestion
Other possible symptoms that occur more often in women include:
-
Abdominal pain
-
Heartburn
-
Clammy skin
-
Severe tiredness
-
Anxiety