A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Cystectomy
Cystectomy is surgery to remove the urinary bladder. It may be done in certain cases of bladder cancer. Your healthcare provider can discuss the risks and benefits of the surgery with you.
Getting ready for surgery
You will be asked to read and sign a form consenting to the surgery. Be sure to read the entire document. Have all of your questions answered before signing it.
You’ll be told how to get ready for surgery. These instructions may include:
-
Donating your own blood a few days before the surgery. This is in case you need a transfusion during the surgery.
-
Taking antibiotics before surgery. This is to help prevent infection.
-
Not eating or drinking anything a certain amount of time before surgery.
-
Clearing your intestine. You may do this by drinking a special liquid at home. Or you may be admitted to the hospital the night before surgery and given medicine and enemas to empty the intestine.
Removing the bladder
The surgery is done in a hospital. It takes about 4 to 6 hours. Just before surgery, you’ll be given medicine to prevent pain (general anesthesia). This allows you to sleep comfortably through the entire procedure. A cut (incision) is then made near your belly button. This exposes the bladder. The area around your bladder is checked to see if the cancer has spread. If it has, the surgery may not be continued. If the cancer is only in the bladder, the bladder is removed. Other organs near the bladder may be removed as well. This is in case cancer cells may have spread to those organs.
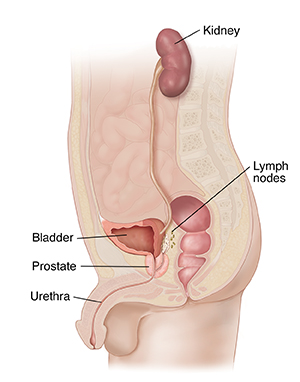 |
| In men, the bladder, lymph nodes, prostate, and often the urethra are removed. |
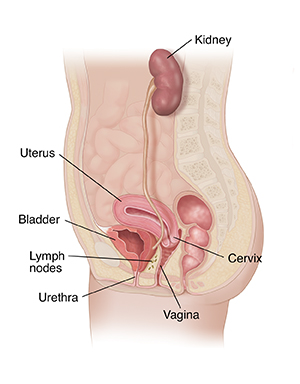 |
| In women, the bladder, uterus, cervix, lymph nodes, urethra, and sometimes part of the vagina are removed. |
Creating a new path for urine
After the bladder is removed, you'll need a new way to store and release urine. There are three different choices. Talk with your healthcare provider about which choice would be best for you. The choices include:
-
Incontinent diversion. A short piece of intestine is removed and connected to the ureters. The other end is connected to the skin on the front of the belly (abdomen). This forms an opening called a stoma. This procedure is called a urostomy. A small bag is placed over the stoma to collect the urine.
-
Continent diversion. A valve is created in a pouch made from a piece of intestine. You can empty the pouch several times a day by putting a drainage tube (catheter) into the stoma through the valve. This method doesn't need a collection bag.
-
Neobladder. A new bladder is made from a piece of intestine and urine is routed back into the urethra, so you pass urine the same way. Over time most people are able to return to normal urination during the day on a schedule. However, incontinence at night may be a problem.
If the cancer can't be removed with surgery, or it has spread, a diversion may be done without taking out the bladder. In this case, the purpose of doing the diversion is to prevent or end the blockage of urine flow instead of curing the cancer.
Risks and possible complications
Possible risks of this procedure include:
-
Infection
-
Bleeding that needs a transfusion
-
Blocked intestine
-
Inability to have an erection or trouble having sex
-
Blood clot in the legs or lungs because of physical inactivity
-
Damage to nearby organs
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
8/1/2023
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.