A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
When Your Child Has Epiglottitis
Epiglottitis is a medical emergency. It’s an infection of the epiglottis. This is the small flap of tissue at the back of the throat. It stops food and liquids from entering the windpipe (trachea) when a person eats or drinks. The rest of the time it lifts, so air can flow easily into and out of the lungs. Epiglottitis causes swelling that may close off the airway and make it hard to breathe. This condition requires medical care right away. If not treated quickly, it can be fatal.
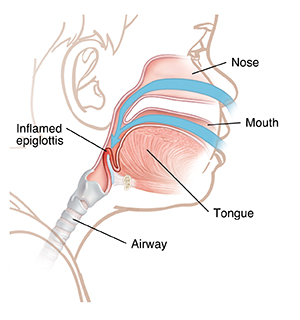 |
| An inflamed epiglottis blocks the airway. |
What causes epiglottitis?
Most often, epiglottitis results from infection with Haemophilus influenzae type b (Hib) bacteria. The bacteria spread through the air in tiny droplets when an infected person coughs or sneezes. The infection starts with a high fever and sore throat. Breathing problems can come on quickly. Now that there is an Hib vaccine, this infection is very rare. Talk with your child's healthcare provider about the Hib vaccine.
Epiglottitis is an emergency!
Call 911
Epiglottitis can be deadly if not treated quickly. If your child has any of the symptoms below, call 911right away:
-
Trouble breathing
-
Trouble swallowing or talking
-
Straining the neck forward (trying to open the airway)
-
Drooling (when it becomes too painful to swallow)
-
A harsh raspy sound when inhaling (stridor), a sign that the airways are blocked
-
Blue, purple, or gray skin or lips
-
Trouble waking up or unresponsive
When the above symptoms occur:
-
Don’t try to check your child’s throat yourself. You may make matters worse.
-
Don’t give your child food, water, or cough medicines. These may cause vomiting and make it even harder to breathe.
-
Don’t encourage your child to lie down. They will likely be the most comfortable leaning forward in a sitting position.
How is epiglottitis treated?
-
To allow air into the lungs, a healthcare provider may place a breathing tube into the windpipe. The tube is passed through your child’s nose or mouth. It provides an airway around the swelling, letting air flow freely into and out of the lungs. The breathing tube must stay in place until the swelling in the throat has gone down.
-
In the most serious cases, a healthcare provider may create an emergency airway into the windpipe directly through a hole in the neck.
-
Once your child is breathing more easily, certain tests may also be done. These may include X-rays, blood tests, and a throat culture. This is a test that looks for bacteria in a sample of material from the throat.
-
Antibiotics and fluids will be given through an IV (intravenous) line.
-
Your child’s breathing will be watched closely.
What are long-term concerns?
With prompt treatment, most children get better with no lasting effects.
The Hib vaccine
Getting the Hib vaccine is the best way to prevent epiglottitis. Talk with your child's healthcare provider right away about getting the vaccine.
Other germs can lead to epiglottitis. But Hib bacteria are the most common cause. Children often get the vaccine at:
Online Medical Reviewer:
Jessica Gotwals BSN MPH
Online Medical Reviewer:
Liora C Adler MD
Online Medical Reviewer:
Marianne Fraser MSN RN
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.