Tuberculosis (TB)
Tuberculosis (TB) is a serious disease caused by germs (bacteria) that spread from person to person through the air. Most often, TB infects the lungs. But it can also affect other parts of the body such as lymph glands, the brain, the kidneys, and the spine. TB is a common cause of death worldwide. Here's more information about TB, how it's treated, and ways to help prevent its spread.
What are the risk factors for TB?
Anyone can get TB. But you may be at greater risk if you:
-
Have an immune system weakened by medicines such as steroids, autoimmune disorders and treatments, or a disease such as HIV infection
-
Have close contact with someone who has untreated active TB of the lungs
-
Are older
-
Live or work in a residential facility, such as a shelter, nursing home, or prison
-
Travel to or come from a country where there are high rates of TB infections, such as India and parts of Asia and Africa
How does TB spread?
TB bacteria are released into the air when someone with the active form of lung TB coughs or sneezes. The bacteria spread easily, especially in crowded places with poor airflow. The longer you breathe these germs, the more likely you are to become infected.
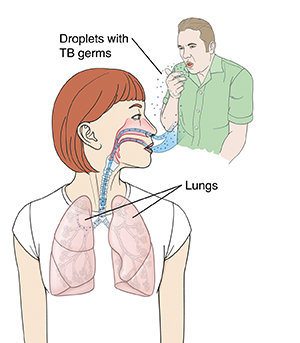 |
| TB germs spread through the air when someone with the active form of TB coughs or sneezes. |
What are the symptoms of TB?
There are 2 types of TB: inactive (also called latent TB infection) and active (also called TB disease).
Inactive TB (latent TB infection)
If you've been diagnosed with inactive TB, it means you:
-
Have live TB bacteria in your lungs, but the germs have been sealed off, much like a scab covers a wound. As a result, you don’t have symptoms or feel sick. The only way to know you have inactive TB is with a TB test.
-
Can’t spread the infection to others
-
Generally need medicine to keep the infection from becoming active at some future time
Active TB (TB disease)
If you've been diagnosed with active TB, it means you:
-
Have symptoms of TB. These include a lasting cough, phlegm, severe tiredness (fatigue), fever, night sweats, swollen glands, and weight loss. There may be other symptoms from the part of the body affected. You're likely to feel very sick.
-
Can spread the infection to others if your active TB affects the lungs or throat
-
Must take medicine to help cure the disease. Treatment takes at least 6 months. TB is sometimes hard to cure.
How is TB diagnosed?
Several tests are used to help find TB infection:
-
Skin test (PPD). A testing solution is placed just under the skin on your arm. This is done to see if there's a reaction (such as a hard, red bump). You'll need to return to the office in 2 or 3 days to have your arm checked. Be sure to keep the appointment. You'll learn the test results during this visit.
-
Blood test. A small amount of blood is drawn and sent to a lab for testing. Your healthcare provider can tell you if this test is offered in your area.
-
Other tests. If you have TB infection, other tests, such as a chest X-ray, are needed to learn if the infection is active. Your provider may also take a sample of the mucus that comes up when you cough (sputum). Your provider may do a biopsy of a swollen gland or other body part. The sample is sent to a lab and tested for TB bacteria. Knowing the type of bacteria causing your illness helps your provider choose the right medicine to treat the disease.
What do the test results mean?
-
A negative result usually means that your body is free of TB bacteria. Sometimes the test can be negative, even in someone with TB infection or active TB.
-
A positive result means you've been exposed to the germs that cause TB. You may have an inactive or active infection. You'll need further evaluation.
How is TB treated?
-
Both inactive and active TB are treated with antibiotic medicines. If you have active TB, you'll be prescribed more medicines for a longer time.
-
You'll likely begin feeling better shortly after starting treatment. But even if you're feeling better, it's important to keep taking all the medicine you've been prescribed. This is the only way to cure the disease. Not taking all the medicine means you won’t get well and can keep spreading TB germs to others.
-
Sometimes TB is drug-resistant. This means it doesn’t respond to one or more of the usual medicines for TB. Resistant TB is harder to cure. It requires different medicines and often longer treatment.
What is DOT?
During treatment, you may be offered or be required to take part in a program called DOT (directly observed therapy). In this program, a nurse or healthcare worker supervises your treatment. This is a standard approach. It makes it easier to manage medicines, watch for any side effects, and make sure the medicines are working.
During treatment for TB
-
Take all the medicine as directed, even when you start feeling better. You'll take the medicine for 6 months or longer. Sticking to this schedule takes patience. But stopping treatment early means your symptoms may come back. It may also lead to drug-resistant TB.
-
Get plenty of rest and eat healthy meals. A nutritious diet full of fresh fruits and vegetables helps the body fight infection.
-
Check with your healthcare provider before using any over-the-counter (OTC) medicines that haven’t been prescribed. OTCs can interact with your prescription medicines.
-
If you're taking birth control pills, you may need to also use a backup method of birth control. Some TB medicines may make the pill less effective.
-
You might need to limit your activity so you don't have fatigue.
-
Keep your medical appointments. You'll need to be checked often to make sure that your medicine is working and you're getting better.
How you can help a loved one with TB
TB is a serious illness that takes a long time to cure. If you have a family member or friend with TB, you can help by reminding your loved one to:
-
Take TB medicines at the same time every day (they’re best taken with water, milk, or juice 30 minutes before meals or at bedtime).
-
Keep all follow-up appointments (you can help by driving or arranging for a ride).
-
Get plenty of rest.
-
Eat healthy meals.
Preventing the spread of TB
If you have active TB of the lungs or throat:
-
Ask family, friends, and the people you work with to get tested. Active TB can spread to other people.
-
Don't have close contact with others until your healthcare provider says it’s OK.
-
Wash your hands often, especially after coughing. Use soap and clear, running water and scrub your hands for at least 20 seconds.
-
Don't touch your eyes, nose, and mouth with unwashed hands.
-
Don't prepare or eat food and drinks with unwashed hands.
-
Don't touch surfaces or objects that have germs on them.
-
Don't blow your nose, cough, or sneeze into your hands and then touch other people’s hands or common objects.
-
Use a tissue to cover your mouth when you cough. If you don’t have a tissue, cough into your elbow, not your hand. Wash your hands after you cough or sneeze.
-
Wear a mask, if you've been told to do so, when you go out in public or visit your healthcare provider.
-
Use a plastic bag to throw away old tissues and other supplies.
When to call the healthcare provider
Call your healthcare provider right away if you have any of the following:
-
A fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Increased coughing or coughing up blood
-
Chest pain or shortness of breath
-
Night sweats that get worse or keep coming back
-
Trouble breathing
Also call your provider if you're taking TB medicine and think you're having side effects. These include skin rash, yellowing of the eyes, or stomach problems.