Understanding an Intrathecal Pain Pump Implant
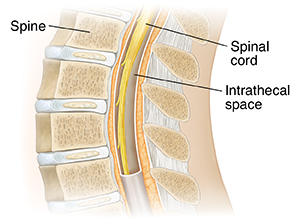
An intrathecal pain pump implant is a way to relieve some kinds of long-term (chronic) pain or cancer pain. It sends pain medicine through a thin, flexible tube. The tube is inserted into the space around the spinal cord. The area between the spinal cord and the tissue (membrane) covering the cord is called the intrathecal space. This space contains a liquid called cerebrospinal fluid (CSF).
The tube is connected to a small, round pump. Both are implanted under your skin in a minor surgery. A small electronic device controls the pump. The device stays outside your body. The pump contains medicine and sends it through the tube into the CSF. The medicine reaches nerves along the spine. It helps prevent them from sending pain signals to the brain.
How to say it
ihn-trah-THEE-kuhl
Why an intrathecal pain pump implant is used
An intrathecal pain pump implant may be used if you have chronic pain or long-term pain such as pain due to cancer, an injury, or a disease. It can help ease pain when other types of pain care have not worked or have caused severe side effects. It may be used after you have tried pain medicine by pill, liquid, or injection. It may also be used if surgery to treat the source of pain is not an option.
How an intrathecal pain pump is implanted
Before having an intrathecal pain pump implanted, this type of pain care is tested to make sure it will work for you. This is called a trial. You may have an injection of pain medicine or a short-term (temporary) test of an intrathecal pain pump. During this procedure:
-
You lie face-down on a medical table. An area in your back over your spine is numbed. You may be given medicine to relax you or make you sleep.
-
The healthcare provider makes a small cut (incision) in your skin over part of your spine. They put a stiff tube through the skin. It goes into the space around the spinal cord (intrathecal space).
-
The provider then puts a thin, flexible tube (catheter) through the first tube and moves it farther into the intrathecal space. Pain medicine is sent through this tube for a few days to see if it helps your pain.
If the pain relief trial works for you, a pump will be implanted. For this procedure:
-
You lie face-down on a medical table. You are given medicine to relax you or make you sleep through the procedure.
-
The healthcare provider removes the first catheter you had. They put a new catheter under your skin.
-
The provider then puts a pump about 1 inch under your skin on one side of your lower belly (abdomen). The pump is a disk about 1 inch thick and 3 inches wide. It contains medicine and has a battery that lasts for 5 to 7 years. The catheter is connected to the pump.
-
The provider connects the pump to a small device outside your body. The provider uses this device to control the pump.
The pump may be programmed by the healthcare provider or set to a certain amount. The type of medicine used in the pump will depend on your type of pain and other factors. The pump will need to be refilled with medicine when needed. This may happen every 1 to 3 months.
Risks of an intrathecal pain pump implant
-
Infection
-
Small growth of tissue near the catheter (granuloma)
-
Mistakes in programming the device that may make the medicine dose too high or too low
-
Tear in the catheter that stops the medicine from getting to nerves
-
Side effects of opioid or other medicine
-
Damage to the nerves on the spine
-
Leaking of cerebrospinal fluid (CSF) that causes headache and other symptoms
-
A pocket of CSF under the skin (hygroma)
-
A pocket of other fluid under the skin (seroma)
-
Changes in endocrine function
-
Need for higher doses of medicine over time
Online Medical Reviewer:
Jessica Gotwals RN BSN MPH
Date Last Reviewed:
8/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.