Having Carotid Angioplasty and Stenting
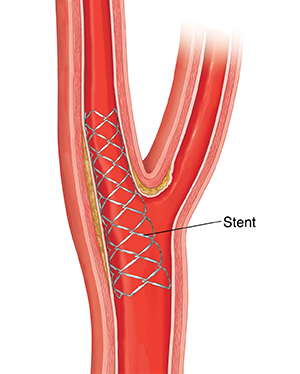
Angioplasty and stenting is a procedure to improve the blood flow in an artery or vein. The carotid arteries are large arteries inside each side of your neck. During the procedure, healthcare providers use a thin tube with a balloon at its tip to open up the artery. This is called angioplasty. A tiny mesh tube called a stent is then put into the artery. It's left in place to help keep the artery open. This is a minimally invasive procedure. It's done with a small cut (incision) usually in your groin.
What to tell your healthcare provider
Before the procedure, make sure to tell the medical team if you:
-
Have had any recent changes in your health, such as a fever
-
Are pregnant or could be
-
Are allergic to shellfish, iodine, or any other substance
-
Have ever had a bad reaction to contrast dye
-
Have ever had a problem with medicine that helps you relax (sedation)
Tests before your procedure
You may need some tests before the procedure, such as:
-
Blood tests, to check for anemia and infection
-
An electrocardiogram (ECG), to check your heart rhythm
-
A chest X-ray, to look at your heart and lungs
-
Ultrasound of your neck, to look at the carotid artery
-
CT angiogram of the blood vessels of your neck and head
Getting ready for your procedure
Talk with your healthcare provider about how to get ready. Tell them about all the medicines you take. This includes over-the-counter medicines such as aspirin, vitamins, and other supplements. You may need to stop taking some medicines, such as blood thinners, ahead of time. If you smoke, you’ll need to stop before your procedure. Nicotine from any source (cigarettes, e-cigarettes, patches, chewing tobacco) slows healing. Talk with your healthcare provider if you need help to stop smoking.
Follow any directions you are given for not eating or drinking before your procedure. Your healthcare provider may give you more instructions about how to get ready.
On the day of your procedure
Talk with your healthcare provider about what to expect. The procedure will likely be done by a healthcare provider trained in vascular medicine and a team of specialized nurses. A typical procedure may go like this:
-
An IV (intravenous) tube will be put in your arm or hand before the procedure starts. You’ll be given sedation through the IV tube. This will make you relaxed and sleepy during the procedure.
-
Hair in the area of your procedure may be removed. The area may be numbed with a local anesthesia.
-
The healthcare provider will make a small incision in a blood vessel in your groin. They will then put a long, thin wire into this cut. The wire acts as a guide during the procedure.
-
The healthcare provider will then insert a thin, flexible tube (catheter) over the wire. It has a tiny deflated balloon on the end. The catheter will be threaded through the blood vessel all the way into the carotid artery in your neck. Continuous X-ray images may be used to show exactly where the catheter is.
-
The healthcare provider will inflate the balloon inside the narrow part of the carotid artery. This will stretch the area open.
-
A mesh tube called a stent may be left in place in the area. This will help keep the area open.
-
The healthcare provider will deflate the balloon and remove the catheter.
-
The healthcare provider will close and bandage the incision site in the groin.

After your procedure
After the procedure, you will spend several hours in a recovery room. You may be sleepy when you wake up. Your healthcare team will watch your heart rate and breathing. You’ll be given pain medicine if you need it.
You may need to lie flat without bending your legs for several hours after the procedure. This is to help prevent bleeding from the incision site. You may be able to go home the same day. Or you may need to stay in the hospital overnight. Your healthcare provider will tell you what to expect. When you’re ready to go home, you’ll need to have a family member or friend drive you.
Recovering at home
Your healthcare provider may prescribe medicines to help prevent blood clots or spasm of your blood vessels. Follow all of your healthcare provider’s instructions. This includes any advice about medicines, exercise, and wound care. The post-procedure medicines are very important. Don't skip or adjust the dose. Call your healthcare provider if you have medicine questions. You may have some pain after the procedure. You may have a bruise and swelling where the catheter was inserted in your groin. You can take over-the-counter pain medicines if you need to. Get some rest. Don't do any strenuous exercise for at least 24 hours.
Follow-up care
If you had symptoms from your carotid stenosis, these should go away after the procedure. In follow-up appointments, your healthcare provider will talk with you about your continued care. This includes ways to lower your risk for atherosclerosis. You also may need follow-up blood tests or imaging of your neck.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38.0°C) or higher, or as advised by your healthcare provider
-
Swelling or pain at the incision site gets worse
-
Fluid or blood leaking from the incision site
-
Redness or warmth at the incision site
-
The limb that was used for the puncture site is cold, painful, numb, tingling, changes color, or has loss of function
-
New symptoms or symptoms get worse
-
Chest pain or trouble breathing (Call 911)
Call 911 right away if you have any of the following symptoms of stroke:
-
Weakness, tingling, or loss of feeling on one side of your face or body
-
Sudden double vision or trouble seeing in one or both eyes
-
Sudden trouble talking or slurred speech
-
Trouble understanding others
-
Sudden, severe headache
-
Dizziness, loss of balance, or a sense of falling
-
Blackouts or seizures
B.E. F.A.S.T. is an easy way to remember the signs of stroke. When you see these signs, you know that you need to call 911 fast.
B.E. F.A.S.T. stands for:
-
B is for balance. Sudden loss of balance or coordination.
-
E is for eyes. Vision changes in one or both eyes.
-
F is for face drooping. One side of the face is drooping or numb. When the person smiles, the smile is uneven.
-
A is for arm weakness. One arm is weak or numb. When the person lifts both arms at the same time, one arm may drift downward.
-
S is for speech difficulty. You may notice slurred speech or trouble speaking. The person can't repeat a simple sentence correctly when asked.
-
T is for time to call 911. If someone shows any of these symptoms, even if they go away, call 911 right away. Make note of the time the symptoms first appeared.