Lung Health for a Child with Cystic Fibrosis
If your child has cystic fibrosis, you need to work closely with your child’s healthcare provider and the rest of the healthcare team. This helps your child to stay healthier, feel better, and have a better quality of life. It also slows the decline in your child’s lung function. Your child’s healthcare provider may suggest many ways to maintain lung health. These include airway clearance therapy (ACT), medicine, nutrition, preventing infection, and exercise.
Airway clearance therapy (ACT)
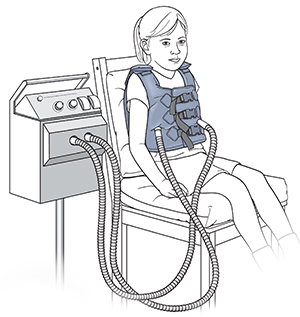 |
| A vibrating vest is an airway clearance device that helps loosen mucus. |
ACT helps loosen and clear mucus from the airways, letting your child breathe better. It may also lower their risk for infection. There are several different ways to do ACT. Work with your child's healthcare provider to figure out the best one for your child.
ACT often includes certain breathing and coughing techniques. Your child may also use a special device to loosen mucus. They may wear a vibrating vest.
Your child may also have chest physical therapy (CPT) to help loosen and clear thick secretions from the lungs. It greatly improves lung function and reduces the amount of lung damage over time. You will work with a physical therapist to learn how to do CPT. CPT often includes 3 methods:
-
Postural drainage. This method places your child’s body in positions that allow mucus to drain.
-
Percussion. This is a clapping method to loosen secretions. An airway clearance device, such as a vibrating vest, is an alternative to manual clapping.
-
Coughing. This is used to help remove lung secretions.
Medicine
 |
| A nebulizer turns medication into a fine mist that your child can breathe in. |
Your child may need medicine to prevent or treat lung problems. Many are taken with a nebulizer. This is a device that turns medicine into a mist that your child can breathe in (inhale). Medicines can include:
-
Antibiotics. These can prevent or treat lung infections. They may need to be used for short periods of time (acute use) or for long periods (chronic use). They may be taken by mouth (oral), inhaled, or given by IV (intravenously).
-
Bronchodilators. These help to open airways.
-
Anti-inflammatory medicines. These help to decrease airway inflammation.
-
Medicines to thin secretions. These include dornase alfa or hypertonic saline.
-
CFTR (cystic fibrosis transmembrane conductance regulator) modulators. These can help improve lung function. They include ivacaftor or lumacaftor. These medicines can help the defective CFTR protein to work correctly. With cystic fibrosis, the CFTR protein does not work well because of changes (mutations) in the CFTR gene. Mucus then becomes thick and sticky. And there are blockages in the lungs and digestive system. Ask your provider if these medicines are right for your child.
-
Oxygen therapy. This may be advised to treat low levels of oxygen in your child's blood when they are participating in physical activities or attending school or work.
-
Nutritional supplements. These may be advised when healthy eating is not enough. They may include calcium, multivitamins, oral pancreatic enzymes, sodium, and vitamins A, D, E, and K.
Nutrition
Improving your child’s nutrition can also improve lung health. It does this by limiting infections. It also helps with other problems related to cystic fibrosis. You will work with your child’s healthcare team to do one or more of the following:
-
Increase the number of calories your child eats.
-
If advised by the healthcare provider, give your child more foods high in antioxidants. These are chemicals that reduce damage from inflammation in the body.
-
Give your child prescribed pancreatic enzymes to help with nutrient absorption.
-
Give your child advised vitamin supplements to replace those not well absorbed from food.
Prevention infection
People with cystic fibrosis are at a higher risk for lung infections. There are several ways to help prevent infections:
-
Vaccines. It is important to remain up-to-date with your child's vaccines. Talk with your child's healthcare provider about what vaccines your child needs. This may include the influenza, COVID-19, and pneumococcal vaccines.
-
Handwashing. This is important for you, your child, and their caregivers. Handwashing can help prevent infections from spreading from one person to another. Wash your hands with soap and clean water for at least 20 seconds. Or use a hand sanitizer with at least 60% alcohol. Be sure to wash your hands after coughing, sneezing, chest physiotherapy, and spending time in public places.
Exercise
Encourage your child to be active. Exercise helps your child stay healthier. It improves your child’s overall condition and helps them feel better both physically and emotionally. It also helps to loosen mucus, which makes it easier to breathe. Talk to your healthcare team about what types of exercise and school sports are safe for your child. If regular school sports programs are not safe for your child, ask about community resources for adaptive exercise and sports programs.
Follow-up care
Your child should see a healthcare provider who is trained in treating cystic fibrosis every 3 months. If a cold or other breathing problem occurs, your child may need to see their healthcare provider more often. Your child can see their regular healthcare provider for minor problems not related to cystic fibrosis.
It's important that all providers are aware of your child's medical condition and recent changes. Update them about new medicines, infections, and routine vaccines.
Be sure to keep all follow-up appointments. In an age-appropriate way, explain cystic fibrosis to your child. Then they can ask providers questions during clinic visits.
When to call your child's healthcare provider
Call the healthcare provider right away if your child has any of the following:
-
More coughing or more sputum
-
Symptoms that get worse, or new symptoms
-
Wheezing
-
Decreased appetite
-
Fever of 100.4° F ( 38°C ) or higher, or as advised by the provider
-
Chest pain or tightness
-
Belly pain
-
Coughing up blood
Call 911
Call 911if your child has any of these:
-
Wheezing that gets worse or doesn't get better after treatment
-
Shortness of breath or trouble breathing
-
Trouble swallowing or talking
-
Chest pain or chest tightness that gets worse or doesn't get better after treatment
-
Blue, purple, or gray skin color
-
Fainting or loss of consciousness