Raynaud Disease
Your healthcare provider has told you that you have Raynaud disease. It's also called Raynaud phenomenon (RP) or Raynaud syndrome. There's no cure for Raynaud disease. But you can manage it to help prevent attacks.
What are the symptoms of Raynaud disease?
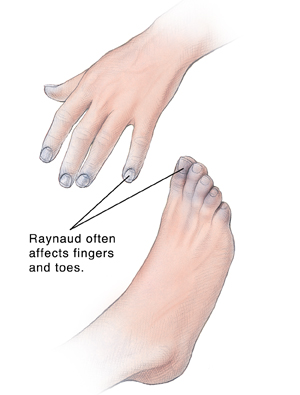
A Raynaud disease attack is often triggered by cold or stress. During an attack, blood vessels suddenly narrow (called vasospasm). This most often happens in fingers and toes. In rare cases, the nose, ears, nipples, or even tongue are affected. Narrowed blood vessels reduce the blood supply to the area. The area then turns white, blue, or red. The area may feel tingling, numb, or painful. As the attack passes, the blood vessels open. The affected area may turn bright red as it warms up, then returns to normal color.
What is the cause of Raynaud disease?
With Raynaud disease, it's believed that blood vessels in the affected areas respond too strongly to certain triggers, such as cold. This makes them narrow (called vasospasm) much more than in people without the disease. Experts don’t know what causes the blood vessels to react so strongly to certain triggers. In between attacks, the blood vessels are normal and healthy. Attacks don’t permanently damage the blood vessels. But they may thicken the artery walls.
In some cases, Raynaud disease happens along with another disease or condition. This is often a connective tissue disorder, such as lupus, scleroderma, or rheumatoid arthritis. This is called secondary Raynaud disease (as opposed to primary Raynaud disease discussed above) and may be more severe. If this is the case for you, you and your healthcare provider can discuss treatment for the underlying condition.
What are the risk factors?
Risk factors for Raynaud disease include:
-
Women are more likely to get Raynaud disease than men.
-
Younger people are at higher risk, often ages 15 to 30.
-
Living in colder climates increases risk.
-
Having a family member with Raynaud disease increases your risk.
-
Underlying rheumatoid conditions may increase your risk.
What are possible triggers?
Triggers for Raynaud disease include:
-
Cold . Even slight temperature changes can cause an attack. This includes walking into the refrigerated section in the food store.
-
Stress. This causes the body to activate certain substances in the blood vessels that tell the vessels to narrow.
-
Caffeine.
-
Smoking. This causes the blood vessels to narrow. It can make the condition worse.
-
Repetitive movements.
-
Certain medicines. These include beta-blockers, migraine medicine, birth control pills, and others.
-
Injury.
-
Emotions. Being startled can cause an attack of RD. That's because the startle reflex releases substances that tell the vessels to narrow.
How is Raynaud disease diagnosed?
Your description of your symptoms, a health history, and a physical exam are often enough for a diagnosis. Blood tests and other tests may be done to see if any underlying conditions are present and rule out other problems.
How is Raynaud disease treated?
There is no known cure for Raynaud disease. But you can learn to manage symptoms and reduce the number and severity of attacks. For most people, staying away from triggers may be enough to limit attacks. Your healthcare provider may advise you to:
-
Take safety steps to help prevent your hands and feet from losing circulation. This includes:
-
Dressing warmly in cold weather.
-
Wearing gloves or mittens when your hands may become cold, such as when you use the refrigerator or freezer.
-
Not keeping the air conditioning at a low temperature in summer.
-
Staying away from stress and caffeine.
-
Exercising regularly. This may reduce the number and severity of attacks.
-
Quitting smoking, if you smoke. Quitting may improve the condition. This is because smoking causes your blood vessels to narrow and reduces blood flow.
-
Soak your hands or feet in warm (not hot) water. Do this at the first sign of an attack. Keep soaking until your skin color returns to normal.
In some people, symptoms are lasting or troubling. For these cases, other treatments are a choice. Your healthcare provider can tell you more about these:
-
Prescription medicines. Some medicines that relax and widen blood vessels, such as calcium channel blockers. These may help ease symptoms.
-
Nerve surgery. This is used for severe cases that don’t respond to other treatments. Surgery removes the nerves around the blood vessels in the hands and feet. Without nerve stimulation, the blood vessels stay more relaxed. They're less likely to become very narrow due to stimuli. Nerves may be blocked using injections in some cases.
If attacks are severe, last for a long time, or occur very often, skin damage and sores (skin ulcers) may result. Controlling attacks can help prevent this.
When to get medical care
The following problems happen rarely, but they can be serious. Call your healthcare provider right away if you notice any of these:
-
Skin infection or sores
-
A finger or toe turns black
-
The skin breaks open on its own
-
A rash
-
A finger or toe joint becomes painful or swollen